天津医药 ›› 2024, Vol. 52 ›› Issue (9): 940-945.doi: 10.11958/20240147
王远珍1,2( ), 魏红艳1,2, 常丽仙1,2, 张映媛2, 刘春云2, 刘立2,△(
), 魏红艳1,2, 常丽仙1,2, 张映媛2, 刘春云2, 刘立2,△( )
)
收稿日期:2024-01-29
修回日期:2024-04-22
出版日期:2024-09-15
发布日期:2024-09-06
通讯作者:
△E-mail:作者简介:王远珍(1998),女,硕士在读,主要从事肝病流行病学研究。E-mail:基金资助:
WANG Yuanzhen1,2( ), WEI Hongyan1,2, CHANG Lixian1,2, ZHANG Yingyuan2, LIU Chunyun2, LIU Li2,△(
), WEI Hongyan1,2, CHANG Lixian1,2, ZHANG Yingyuan2, LIU Chunyun2, LIU Li2,△( )
)
Received:2024-01-29
Revised:2024-04-22
Published:2024-09-15
Online:2024-09-06
Contact:
△E-mail:王远珍, 魏红艳, 常丽仙, 张映媛, 刘春云, 刘立. 原发性肝癌干预前并发肺部感染风险预测模型的建立与验证[J]. 天津医药, 2024, 52(9): 940-945.
WANG Yuanzhen, WEI Hongyan, CHANG Lixian, ZHANG Yingyuan, LIU Chunyun, LIU Li. Establishment and validation of a risk prediction model for primary liver cancer complicated with pulmonary infection before intervention[J]. Tianjin Medical Journal, 2024, 52(9): 940-945.
摘要:
目的 分析原发性肝癌(PHC)患者干预前合并肺部感染的影响因素,建立列线图风险预测模型并进行验证。方法 选取首次确诊并住院的PHC患者1 635例,依据是否合并肺部感染分为感染组197例和非感染组1 438例。收集患者的体质量指数(BMI)、慢性乙型肝炎(CHB)、慢性丙型肝炎(CHC)、巴塞罗那分期(BCLC)等一般资料,白细胞(WBC)、中性粒细胞(NEU)、血红蛋白(Hb)等血液常规指标,总蛋白(TP)、前白蛋白(PA)、天冬氨酸转氨酶(AST)、γ谷氨酰转移酶(GGT)、碱性磷脂酶(ALP)、异常凝血酶原(PIVKA-Ⅱ)、甲胎蛋白(AFP)、癌胚抗原(CEA)、降钙素原(PCT)、超敏C反应蛋白(hs-CRP)、胆碱酯酶(ChE)、总胆固醇(TC)等血液生化指标,CD3细胞计数(CD3+)、CD4细胞计数(CD4+)、CD4/CD8比值(CD4+/CD8+)、CD19细胞计数(CD19+),白细胞介素(IL)-2、干扰素(IFN)-α、肿瘤坏死因子(TNF)-α等细胞因子。采用单因素分析和Lasso回归筛选变量后使用二元Logistic回归分析确定PHC患者干预前发生肺部感染的危险因素,建立并评价列线图风险预测模型。结果 与非感染组比较,感染组的年龄、吸烟比例、CHC、胸腔积液、胃肠道出血、Child-Pugh分级C级、BCLC A期/C期/D期比例、WBC、NEU、AST、GGT、ALP、PIVKA-Ⅱ、AFP、CEA、PCT、hs-CRP、IL-2、IL-5、IL-6、IL-8、IL-10、IL-12、IFN-γ、TNF-α水平较高,BMI水平、CHB比例、Hb、TP、PA、ChE、TC、CD3+、CD4+、CD4+/CD8+、CD19+、IFN-α水平较低(P<0.05)。Lasso回归和二元Logistic回归分析显示胸腔积液、胃肠道出血,较高水平的年龄、WBC、Hb,较低水平的TP是PHC患者干预前并发肺部感染的独立危险因素,据此建立的列线图模型受试者工作特征(ROC)曲线下面积为0.700(95%CI:0.659~0.740),Hosmer-Lemeshow检验结果示模型拟合优度较好,自抽样法重复抽样1 000次进行内部验证,模型的一致性较好。结论 胸腔积液,胃肠道出血,年龄较大,WBC、Hb水平较高以及较低水平的TP是PHC患者干预前并发肺部感染的独立危险因素,建立的列线图预测模型可有效评估PHC患者干预前发生肺部感染的风险。
中图分类号:
| 组别 | n | 男性 | 年龄/岁 | BMI/(kg/m2) | 饮酒 | 吸烟 | CHB | CHC | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 1 226(85.3) | 54.70±10.63 | 22.67±3.25 | 685(47.6) | 769(53.5) | 1 028(71.5) | 279(19.4) | |||||
| 感染组 | 197 | 172(87.3) | 56.98±10.86 | 22.11±2.84 | 106(53.8) | 125(63.5) | 123(62.4) | 51(25.9) | |||||
| χ2或t | 0.589 | 2.812** | 2.311* | 2.642 | 6.956** | 6.812** | 4.525* | ||||||
| 组别 | 高血压 | 糖尿病 | 胸腔积液 | 胃肠道出血 | Child-Pugh分级(A/B/C) | BCLC分期(0/A/B/C/D) | |||||||
| 非感染组 | 252(17.5) | 208(14.5) | 96(6.7) | 72(5.0) | 584/563/291 | 440/45/542/136/275 | |||||||
| 感染组 | 31(15.7) | 37(18.8) | 47(23.9) | 22(11.2) | 45/73/79 | 34/9/51/31/72 | |||||||
| χ2 | 0.387 | 2.535 | 64.089** | 12.135** | 44.630** | 49.849** | |||||||
表1 2组一般资料比较
Tab.1 Comparison of general information between two groups of patients
| 组别 | n | 男性 | 年龄/岁 | BMI/(kg/m2) | 饮酒 | 吸烟 | CHB | CHC | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 1 226(85.3) | 54.70±10.63 | 22.67±3.25 | 685(47.6) | 769(53.5) | 1 028(71.5) | 279(19.4) | |||||
| 感染组 | 197 | 172(87.3) | 56.98±10.86 | 22.11±2.84 | 106(53.8) | 125(63.5) | 123(62.4) | 51(25.9) | |||||
| χ2或t | 0.589 | 2.812** | 2.311* | 2.642 | 6.956** | 6.812** | 4.525* | ||||||
| 组别 | 高血压 | 糖尿病 | 胸腔积液 | 胃肠道出血 | Child-Pugh分级(A/B/C) | BCLC分期(0/A/B/C/D) | |||||||
| 非感染组 | 252(17.5) | 208(14.5) | 96(6.7) | 72(5.0) | 584/563/291 | 440/45/542/136/275 | |||||||
| 感染组 | 31(15.7) | 37(18.8) | 47(23.9) | 22(11.2) | 45/73/79 | 34/9/51/31/72 | |||||||
| χ2 | 0.387 | 2.535 | 64.089** | 12.135** | 44.630** | 49.849** | |||||||
| 组别 | n | WBC/(×109/L) | NEU/(×109/L) | Hb/(g/L) | PLT/(×109/L) | FIB/(g/L) |
|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 4.83(3.56,6.44) | 3.00(2.09,4.42) | 131.75±31.43 | 108.00(73.00,165.00) | 2.74(2.06,3.62) |
| 感染组 | 197 | 5.84(4.21,7.87) | 4.07(2.59,6.20) | 126.01±29.72 | 114.00(67.50,194.50) | 2.67(1.86,3.76) |
| Z或t | 5.210** | 6.151** | 2.420* | 0.899 | 0.787 |
表2 2组患者血液常规指标比较
Tab.2 Comparison of blood routine indexes between the two groups of patients
| 组别 | n | WBC/(×109/L) | NEU/(×109/L) | Hb/(g/L) | PLT/(×109/L) | FIB/(g/L) |
|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 4.83(3.56,6.44) | 3.00(2.09,4.42) | 131.75±31.43 | 108.00(73.00,165.00) | 2.74(2.06,3.62) |
| 感染组 | 197 | 5.84(4.21,7.87) | 4.07(2.59,6.20) | 126.01±29.72 | 114.00(67.50,194.50) | 2.67(1.86,3.76) |
| Z或t | 5.210** | 6.151** | 2.420* | 0.899 | 0.787 |
| 组别 | n | TP/(g/L) | PA/(mg/L) | AST/(U/L) | ALT/(U/L) | GGT/(U/L) | ALP/(U/L) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 66.41±8.08 | 116.00(76.10,175.55) | 55.00(35.00,101.00) | 37.00(24.00,61.00) | 100.00(50.00,219.00) | 151.50(110.00,228.00) | ||||||||||||||
| 感染组 | 197 | 62.80±8.80 | 94.60(63.75,130.84) | 70.00(39.00,119.50) | 40.00(23.00,69.50) | 137.00(62.00,293.50) | 183.00(126.00,302.00) | ||||||||||||||
| Z或t | 5.803** | 5.263** | 3.189** | 0.415 | 2.794** | 3.936** | |||||||||||||||
| 组别 | PIVKA-Ⅱ/(×103 mAU/L) | AFP/(μg/L) | CEA/(μg/L) | PCT/(μg/L) | SAA/(mg/L) | hs-CRP/(mg/L) | |||||||||||||||
| 非感染组 | 205.50(31.00,3 816.00) | 23.09(4.58,717.85) | 3.04(2.03,4.50) | 0.16(0.07,0.36) | 21.90(6.24,70.16) | 7.72(1.67,26.75) | |||||||||||||||
| 感染组 | 1 566.60(129.70,13 236.00) | 68.73(6.62,5 147.50) | 3.67(2.11,6.15) | 0.29(0.12,0.78) | 30.84(7.28,79.95) | 20.34(7.87,51.76) | |||||||||||||||
| Z | 5.851** | 3.157** | 3.259** | 5.947** | 1.935 | 6.803** | |||||||||||||||
| 组别 | ChE/(U/L) | Cr/(μmol/L) | UA/(μmol/L) | TC/(mmol/L) | TG/(mmol/L) | LDL-C/(mmol/L) | |||||||||||||||
| 非感染组 | 4 011.50(2 539.25,5 992.50) | 65.10(56.00,78.00) | 325.00(254.00,400.25) | 3.79(3.07,4.57) | 1.07±0.79 | 2.33(1.77,3.00) | |||||||||||||||
| 感染组 | 2 921.00(1 797.50,4 554.00) | 67.00(57.00,87.00) | 322.00(255.00,420.00) | 3.54(2.79,4.53) | 1.10±0.79 | 2.28(1.60,3.25) | |||||||||||||||
| Z或t | 6.431** | 1.944 | 0.677 | 2.455* | 0.479 | 0.477 | |||||||||||||||
表3 2组患者血液生化指标比较
Tab.3 Comparison of blood biochemical indexes between the two groups
| 组别 | n | TP/(g/L) | PA/(mg/L) | AST/(U/L) | ALT/(U/L) | GGT/(U/L) | ALP/(U/L) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 66.41±8.08 | 116.00(76.10,175.55) | 55.00(35.00,101.00) | 37.00(24.00,61.00) | 100.00(50.00,219.00) | 151.50(110.00,228.00) | ||||||||||||||
| 感染组 | 197 | 62.80±8.80 | 94.60(63.75,130.84) | 70.00(39.00,119.50) | 40.00(23.00,69.50) | 137.00(62.00,293.50) | 183.00(126.00,302.00) | ||||||||||||||
| Z或t | 5.803** | 5.263** | 3.189** | 0.415 | 2.794** | 3.936** | |||||||||||||||
| 组别 | PIVKA-Ⅱ/(×103 mAU/L) | AFP/(μg/L) | CEA/(μg/L) | PCT/(μg/L) | SAA/(mg/L) | hs-CRP/(mg/L) | |||||||||||||||
| 非感染组 | 205.50(31.00,3 816.00) | 23.09(4.58,717.85) | 3.04(2.03,4.50) | 0.16(0.07,0.36) | 21.90(6.24,70.16) | 7.72(1.67,26.75) | |||||||||||||||
| 感染组 | 1 566.60(129.70,13 236.00) | 68.73(6.62,5 147.50) | 3.67(2.11,6.15) | 0.29(0.12,0.78) | 30.84(7.28,79.95) | 20.34(7.87,51.76) | |||||||||||||||
| Z | 5.851** | 3.157** | 3.259** | 5.947** | 1.935 | 6.803** | |||||||||||||||
| 组别 | ChE/(U/L) | Cr/(μmol/L) | UA/(μmol/L) | TC/(mmol/L) | TG/(mmol/L) | LDL-C/(mmol/L) | |||||||||||||||
| 非感染组 | 4 011.50(2 539.25,5 992.50) | 65.10(56.00,78.00) | 325.00(254.00,400.25) | 3.79(3.07,4.57) | 1.07±0.79 | 2.33(1.77,3.00) | |||||||||||||||
| 感染组 | 2 921.00(1 797.50,4 554.00) | 67.00(57.00,87.00) | 322.00(255.00,420.00) | 3.54(2.79,4.53) | 1.10±0.79 | 2.28(1.60,3.25) | |||||||||||||||
| Z或t | 6.431** | 1.944 | 0.677 | 2.455* | 0.479 | 0.477 | |||||||||||||||
| 组别 | n | CD3+/(×106个/L) | CD4+/(×106个/L) | CD8+/(×106个/L) | CD4+/CD8+ | CD19+/(×106个/L) |
|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 827.89±363.27 | 470.35±215.24 | 302.98±181.58 | 1.87(1.43,2.47) | 138.90(108.29,179.44) |
| 感染组 | 197 | 751.23±332.89 | 422.23±203.70 | 278.73±174.19 | 1.77(1.33,2.23) | 126.35(94.90,175.18) |
| Z或t | 2.805** | 2.961** | 1.767 | 2.066* | 2.579* |
表4 2组患者淋巴细胞计数比较
Tab.4 Comparison of lymphocyte counts between two groups of patients
| 组别 | n | CD3+/(×106个/L) | CD4+/(×106个/L) | CD8+/(×106个/L) | CD4+/CD8+ | CD19+/(×106个/L) |
|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 827.89±363.27 | 470.35±215.24 | 302.98±181.58 | 1.87(1.43,2.47) | 138.90(108.29,179.44) |
| 感染组 | 197 | 751.23±332.89 | 422.23±203.70 | 278.73±174.19 | 1.77(1.33,2.23) | 126.35(94.90,175.18) |
| Z或t | 2.805** | 2.961** | 1.767 | 2.066* | 2.579* |
| 组别 | n | IL-2 | IL-5 | IL-6 | IL-8 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 0.97(0.71,1.36) | 1.39(1.05,2.19) | 22.45(8.52,48.03) | 48.26(32.39,92.34) | |||||
| 感染组 | 197 | 1.14(0.77,1.48) | 1.78(1.25,3.13) | 36.57(16.02,78.28) | 51.81(35.62,115.31) | |||||
| Z | 2.728** | 5.507** | 5.191** | 2.292* | ||||||
| 组别 | IL-10 | IL-12 | IFN-α | IFN-γ | TNF-α | |||||
| 非感染组 | 3.37(2.61,4.69) | 1.96(1.59,2.59) | 56.52(5.07,102.90) | 5.43(3.15,9.22) | 1.70(1.14,4.68) | |||||
| 感染组 | 4.19(2.93,5.85) | 2.22(1.74,5.20) | 32.30(5.19,70.83) | 5.82(3.47,11.45) | 2.66(1.30,9.23) | |||||
| Z | 5.069** | 4.207** | 2.675** | 2.249* | 3.884** | |||||
表5 2组患者细胞因子水平比较 [ng/L,M(P25,P75)]
Tab.5 Comparison of cytokines between two groups of patients
| 组别 | n | IL-2 | IL-5 | IL-6 | IL-8 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 非感染组 | 1 438 | 0.97(0.71,1.36) | 1.39(1.05,2.19) | 22.45(8.52,48.03) | 48.26(32.39,92.34) | |||||
| 感染组 | 197 | 1.14(0.77,1.48) | 1.78(1.25,3.13) | 36.57(16.02,78.28) | 51.81(35.62,115.31) | |||||
| Z | 2.728** | 5.507** | 5.191** | 2.292* | ||||||
| 组别 | IL-10 | IL-12 | IFN-α | IFN-γ | TNF-α | |||||
| 非感染组 | 3.37(2.61,4.69) | 1.96(1.59,2.59) | 56.52(5.07,102.90) | 5.43(3.15,9.22) | 1.70(1.14,4.68) | |||||
| 感染组 | 4.19(2.93,5.85) | 2.22(1.74,5.20) | 32.30(5.19,70.83) | 5.82(3.47,11.45) | 2.66(1.30,9.23) | |||||
| Z | 5.069** | 4.207** | 2.675** | 2.249* | 3.884** | |||||
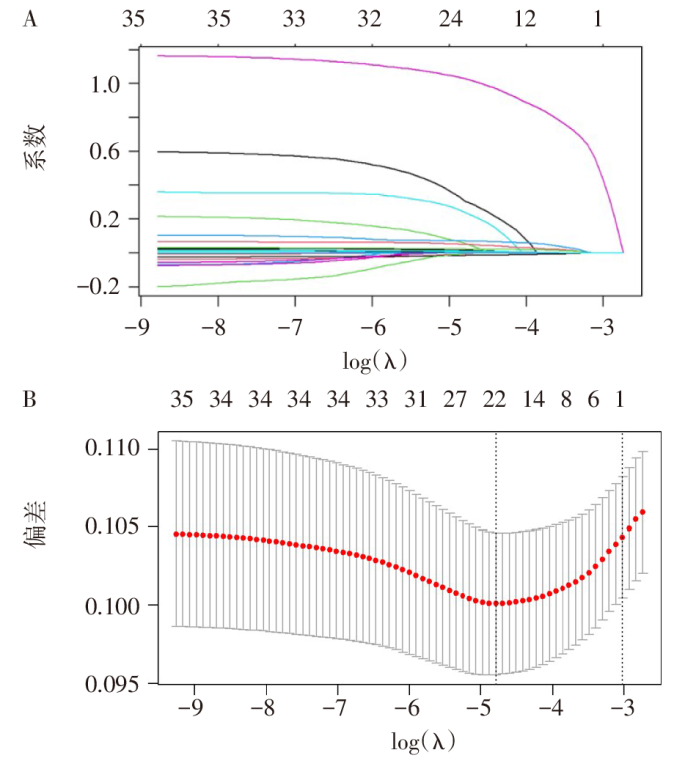
图1 原发性肝癌干预前并发肺部感染的Lasso回归模型 A:系数筛选图;B:变量系数图。
Fig.1 Lasso regression model of pulmonary infection complicated by primary liver cancer before intervention
| 变量 | β | SE | Wald χ2 | P | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.024 | 0.008 | 8.300 | 0.004 | 1.025(1.008~1.042) |
| 胸腔积液 | 1.184 | 0.224 | 27.895 | <0.001 | 3.268(2.106~5.072) |
| 胃肠道出血 | 0.677 | 0.293 | 5.362 | 0.021 | 1.969(1.110~3.493) |
| WBC | 0.069 | 0.032 | 4.807 | 0.028 | 1.072(1.007~1.140) |
| Hb | 0.009 | 0.003 | 6.439 | 0.011 | 1.009(1.002~1.016) |
| TP | -0.024 | 0.011 | 4.449 | 0.035 | 0.976(0.954~0.998) |
| 常量 | -2.261 | 1.164 | 3.772 | 0.052 | 0.104 |
表6 Logistic回归分析原发性肝癌患者干预前并发肺部感染影响因素
Tab.6 Logistic analysis of risk factors for pulmonary infection in patients with primary liver cancer before intervention
| 变量 | β | SE | Wald χ2 | P | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.024 | 0.008 | 8.300 | 0.004 | 1.025(1.008~1.042) |
| 胸腔积液 | 1.184 | 0.224 | 27.895 | <0.001 | 3.268(2.106~5.072) |
| 胃肠道出血 | 0.677 | 0.293 | 5.362 | 0.021 | 1.969(1.110~3.493) |
| WBC | 0.069 | 0.032 | 4.807 | 0.028 | 1.072(1.007~1.140) |
| Hb | 0.009 | 0.003 | 6.439 | 0.011 | 1.009(1.002~1.016) |
| TP | -0.024 | 0.011 | 4.449 | 0.035 | 0.976(0.954~0.998) |
| 常量 | -2.261 | 1.164 | 3.772 | 0.052 | 0.104 |
| 变量 | AUC(95%CI) | 敏感度 | 特异度 | 截断值 |
|---|---|---|---|---|
| 年龄 | 0.554(0.511~0.597) | 0.604 | 0.480 | 53.50岁 |
| 胸腔积液 | 0.586(0.540~0.632) | 0.239 | 0.933 | - |
| 胃肠道出血 | 0.531(0.486~0.575) | 0.112 | 0.950 | - |
| WBC | 0.614(0.572~0.657) | 0.406 | 0.795 | 6.85×109/L |
| Hb | 0.568(0.526~0.610) | 0.604 | 0.543 | 133.50 g/L |
| TP | 0.630(0.587~0.672) | 0.741 | 0.497 | 67.05 g/L |
| 预测模型 | 0.700(0.659~0.740) | 0.563 | 0.784 | - |
表7 各个变量及预测模型评估原发性肝癌干预前发生肺部感染的价值分析
Tab.7 Analysis of each variable and predictive model in evaluating pulmonary infection before intervention of primary liver cancer
| 变量 | AUC(95%CI) | 敏感度 | 特异度 | 截断值 |
|---|---|---|---|---|
| 年龄 | 0.554(0.511~0.597) | 0.604 | 0.480 | 53.50岁 |
| 胸腔积液 | 0.586(0.540~0.632) | 0.239 | 0.933 | - |
| 胃肠道出血 | 0.531(0.486~0.575) | 0.112 | 0.950 | - |
| WBC | 0.614(0.572~0.657) | 0.406 | 0.795 | 6.85×109/L |
| Hb | 0.568(0.526~0.610) | 0.604 | 0.543 | 133.50 g/L |
| TP | 0.630(0.587~0.672) | 0.741 | 0.497 | 67.05 g/L |
| 预测模型 | 0.700(0.659~0.740) | 0.563 | 0.784 | - |
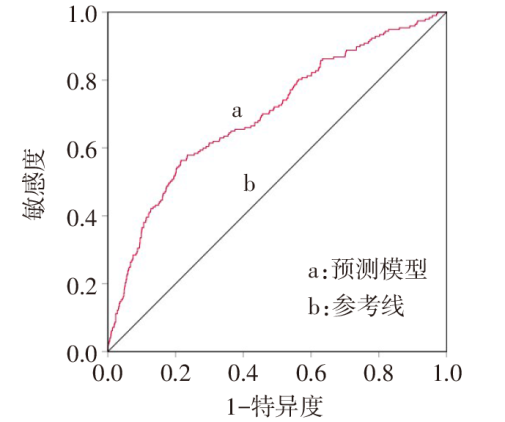
图3 列线图模型预测原发性肝癌干预前发生肺部感染的ROC曲线
Fig.3 A nomogram model predicted the ROC curve of predicting pulmonary infection before intervention in primary liver cancer
| [1] | DRAŠKOVIČ T, ZIDAR N, HAUPTMAN N. Circulating tumor DNA methylation biomarkers for characterization and determination of the cancer origin in malignant liver tumors[J]. Cancers(Basel), 2023, 15(3):859. doi:10.3390/cancers15030859. |
| [2] | RUMGAY H, ARNOLD M, FERLAY J, et al. Global burden of primary liver cancer in 2020 and predictions to 2040[J]. J Hepatol, 2022, 77(6):1598-1606. doi:10.1016/j.jhep.2022.08.021. |
| [3] | ZHOU M, WANG H, ZENG X, et al. Mortality,morbidity,and risk factors in China and its provinces,1990-2017:a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2019, 394(10204):1145-1158. doi:10.1016/S0140-6736(19)30427-1. |
| [4] | MEYERHOLZ D K, BECK A P. Histopathologic evaluation and scoring of viral lung infection[J]. Methods Mol Biol, 2020,2099:205-220. doi:10.1007/978-1-0716-0211-9_16. |
| [5] | YANG L, XU X, LIU Q. Establishment of a risk prediction model for pulmonary infection in patients with advanced cancer[J]. Appl Bionics Biomech, 2022,2022:6149884. doi:10.1155/2022/6149884. |
| [6] | MA Y, TAN B, WANG S, et al. Influencing factors and predictive model of postoperative infection in patients with primary hepatic carcinoma[J]. BMC Gastroenterol, 2023, 23(1):123. doi:10.1186/s12876-023-02713-7. |
| [7] | 王益卓, 刘唯佳, 卢兵, 等. 原发性肝癌合并肺部感染58例临床特征分析[J]. 中华肺部疾病杂志(电子版), 2020, 13(1):83-84. |
| WANG Y Z, LIU W J, LU B, et al. Clinical characteristics analysis of 58 cases of primary liver cancer complicated with pulmonary infection[J]. Chinese Journal of Lung Diseases(Electronic Edition), 2020, 13(1):83-84. doi:10.3877/cma.j.issn.1674-6902.2020.01.019. | |
| [8] | 李伏超, 潘颖, 赵燕, 等. 老年住院患者肺部感染预后相关因素分析[J]. 皖南医学院学报, 2019, 38(1):53-56. |
| LI F C, PAN Y, ZHAO Y, et al. Analysis on the prognostic factors in elderly inpatients with pulmonary infection[J]. Acta Academiae Medicinae Wannan, 2019, 38(1):53-56. doi:10.3969/j.issn.1002-0217.2019.01.015. | |
| [9] | 任锐, 王伟, 陆昌友. 肝癌患者肝切除术后合并肺部感染的现状及相关因素分析[J]. 癌症进展, 2018, 16(2):245-247. |
| REN R, WANG W, LU C Y. Analysis of pulmonary infection status and related factors after liver resection in patients with hepatocellular carcinoma[J]. Oncology Progress, 2018, 16(2):245-247. doi:10.11877/j.issn.1672-1535.2018.16.02.32. | |
| [10] | 张敏龄, 黄津. 老年2型糖尿病合并肺部感染的相关危险因素分析[J]. 临床合理用药杂志, 2021, 14(15):10-12. |
| ZHANG M L, HUANG J. Analysis of risk factors associated with pulmonary infection in elderly patients with type 2 diabetes[J]. Chinese Journal of Clinical Rational Drug Use, 2021, 14(15):10-12. doi:10.15887/j.cnki.13-1389/r.2021.15.004. | |
| [11] | 文静, 贾哲, 赫嵘, 等. 肝细胞癌合并肝硬化门静脉高压症腹腔镜同期联合手术术后肺部感染的危险因素分析[J]. 临床肝胆病杂志, 2023, 39(7):1586-1591. |
| WEN J, JIA Z, HE R, et al. Risk factors for pulmonary infection after laparoscopic surgery in treatment of hepatocellular carcinoma with liver cirrhosis and portal hypertension[J]. Journal of Clinical Hepatology, 2023, 39(7):1586-1591. doi:10.3969/j.issn.1001-5256.2023.07.012. | |
| [12] | 王月平, 赵国厚, 尹飞飞, 等. 终末期肝病患者并发肺部感染的危险因素[J]. 国际呼吸杂志, 2023, 43(9):1041-1045. |
| WANG Y P, ZHAO G H, YIN F F, et al. Risk factors of pulmonary infection in patients with end-stage liver disease[J]. International Journal of Respiration, 2023, 43(9):1041-1045. doi:10.3760/cma.j.cn131368-20221013-00970. | |
| [13] | 刘欣, 李丽. 原发性肝癌患者体液变化的研究[J]. 天津医药, 2021, 49(7):756-759. |
| LIU X, LI L. The study on changes of body fluid in patients with primary liver cancer[J]. Tianjin Med J, 2021, 49(7):756-759. doi:10.11958/20203264. | |
| [14] | 杨惟明, 周鑫, 肖滨增, 等. 老年肝癌伴肝硬化病人上消化道出血的高危因素分析[J]. 实用老年医学, 2020, 34(6):565-568. |
| YANG W M, ZHOU X, XIAO B Z, et al. Risk factors of upper gastrointestinal bleeding in elderly patients with liver cancer complicated with cirrhosis[J]. Practical Geriatrics, 2020, 34(6):565-568. doi:10.3969/j.issn.1003-9198.2020.06.013. | |
| [15] | WU C K, YANG S C, LIANG C M, et al. The role of antibiotics in upper gastrointestinal bleeding among cirrhotic patients without major complications after endoscopic hemostasis[J]. J Gastroenterol Hepatol, 2020, 35(5):777-787. doi:10.1111/jgh.14873. |
| [16] | 毕宁, 安小梅, 王菁, 等. 急性上消化道出血患者发生肺部感染的临床特点及危险因素分析[J]. 中国现代医生, 2021, 59(28):59-62. |
| BI N, AN X M, WANG J, et al. Analysis on the clinical characteristics and risk factors of pulmonary infection in patients with acute upper gastrointestinal bleeding[J]. China Modern Doctor, 2021, 59(28):59-62. | |
| [17] | JIA P, MAO Y, LIU K, et al. The value of color doppler ultrasound and CT combined with serum AFP examination in the diagnosis of hepatocellular carcinoma[J]. J Healthc Eng, 2022,2022:4147753. doi:10.1155/2022/4147753. |
| [18] | AN L, WIRTH U, KOCH D, et al. The role of gut-derived lipopolysaccharides and the intestinal barrier in fatty liver diseases[J]. J Gastrointest Surg, 2022, 26(3):671-683. doi:10.1007/s11605-021-05188-7. |
| [19] | TAJIRI K, OKADA K, ITO H, et al. Long term changes in thrombocytopenia and leucopenia after HCV eradication with direct-acting antivirals[J]. BMC Gastroenterol, 2023, 23(1):182. doi:10.1186/s12876-023-02829-w. |
| [20] | VINER E, BERGER J, BENGUALID V. Etiologies of extreme leukocytosis[J]. Cureus, 2023, 15(4):e38062. doi:10.7759/cureus.38062. |
| [21] | 陶琳. 原发性肝癌患者化疗后抗菌药物的应用及继发感染的危险因素分析[J]. 陕西医学杂志, 2023, 52(1):89-92. |
| TAO L. Application of antibiotics and risk factors of secondary infection in patients with primary liver cancer after chemotherapy[J]. Shaanxi Medical Journal, 2023, 52(1):89-92. doi:10.3969/j.issn.1000-7377.2023.01.021. | |
| [22] | 崔丽娜, 魏昌伟, 吴丹, 等. 肝移植手术后肺部感染的危险因素分析[J]. 临床麻醉学杂志, 2024, 40(1):13-17. |
| CUI L N, WEI C W, WU D, et al. Risk factors for postoperative pulmonary infection undergoing liver transplantation[J]. Journal of Clinical Anesthesiology, 2024, 40(1):13-17. doi:10.12089/jca.2024.01.003. | |
| [23] | SENSUI M, YASUI S, OGASAWARA S, et al. Liver cirrhosis is a risk factor for poor prognosis of acute cholangitis caused by choledocholithiasis[J]. Ann Hepatol, 2022, 27(3):100696. doi:10.1016/j.aohep.2022.100696. |
| [24] | 任华琼, 钟珊, 雷宇, 等. 失代偿期肝硬化并发败血症的危险因素分析[J]. 中华肝脏病杂志, 2022, 30(11):1163-1169. |
| REN H Q, ZHONG S, LEI Y, et al. Analysis of risk factors for decompensated cirrhosis complicated with sepsis[J]. Chinese Journal of Hepatology, 2022, 30(11):1163-1169. doi:10.3760/cma.j.cn501113-20210913-00469. |
| [1] | 郭振江, 赵光远, 杜立强, 刘防震. 近端胃癌上切缘阳性术前列线图预测模型的建立和验证[J]. 天津医药, 2024, 52(8): 845-849. |
| [2] | 王磊, 孟坤, 王兵. 支气管肺炎患儿反复喘息的影响因素分析及预测模型构建[J]. 天津医药, 2024, 52(8): 850-853. |
| [3] | 吴静, 范志娟, 刘树业. 慢性乙型肝炎发展为肝细胞癌过程中血浆游离氨基酸水平的变化及临床意义[J]. 天津医药, 2024, 52(7): 738-742. |
| [4] | 薛玉恒, 茆宁, 刘文强, 杨倩倩, 徐艳, 王军. 基于早期血小板相关参数的支气管肺发育不良风险预测模型的构建与验证[J]. 天津医药, 2024, 52(7): 748-754. |
| [5] | 王敏, 王龙胜, 陈磊. 骨质疏松症患者腰椎骨折预测模型的构建[J]. 天津医药, 2024, 52(7): 766-769. |
| [6] | 韩琴, 韩秀丽, 陈伟然. 老年脑卒中患者康复治疗后抑郁障碍的影响因素分析[J]. 天津医药, 2024, 52(6): 639-642. |
| [7] | 刘小艳, 卜锐, 陆健斐, 丁昱, 张幸. 术前Sonazoid超声造影评估肝细胞癌病理分化程度的价值[J]. 天津医药, 2024, 52(6): 658-662. |
| [8] | 郑康鹏, 唐鑫国, 徐琦, 樊钰亭, 梁博, 付晓伟, 方路. 胆囊癌根治手术成功实施列线图预测模型的建立和验证[J]. 天津医药, 2024, 52(5): 536-540. |
| [9] | 徐杨, 袁宇, 高金妹. 超声检查对骨折患者下肢深静脉漂浮血栓脱落的诊断意义[J]. 天津医药, 2024, 52(5): 548-551. |
| [10] | 冯李婷, 李莉, 谢鑫, 王星. 天津地区部分居民慢性阻塞性肺疾病影响因素分析[J]. 天津医药, 2024, 52(4): 427-431. |
| [11] | 纪晓娟, 韩浩, 张丽侠. 急性髓系白血病合并血流感染的病原菌分布与耐药性变迁及患者死亡的危险因素分析[J]. 天津医药, 2024, 52(2): 167-171. |
| [12] | 孙瑞雪, 刘霄霄, 岳欣怡, 杨冬梅, 任鲁宁, 王菲, 杜红阳. 术前血液学炎症指标对基底细胞癌复发风险的预测价值[J]. 天津医药, 2024, 52(12): 1274-1277. |
| [13] | 谷巍, 张惠娜, 侯丽萍, 于敏, 程黎蓉. 脂质相关指数与糖尿病肾病相关性研究[J]. 天津医药, 2024, 52(12): 1308-1312. |
| [14] | 喻萍, 周敏, 苏丹. 卵巢癌化疗耐药预测模型的建立及效果评价[J]. 天津医药, 2024, 52(11): 1177-1182. |
| [15] | 梁耀冰, 符振华, 赵梓粤, 罗剑明, 程冬瑀, 姜海行, 覃山羽. 高甘油三酯血症性急性胰腺炎并发急性呼吸衰竭危险因素及预测模型的建立[J]. 天津医药, 2024, 52(11): 1183-1187. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||